Payor Authorization Exemption Programs – A Summary and Impact Review
In the past 18 months, insurance providers have sought opportunities to counter the push back on prior authorization processes that have been criticized by insureds, providers, politicians and media outlets.
While insurers argue that authorizations help reduce costs and avoid unnecessary care, providers and patients have argued that it creates artificial barriers to treatment and diagnostics.
To combat this criticism, many payors are either reducing the number of codes that require authorizations, or more recently, are offering programs that exempt providers from authorization requirements if they meet certain criteria.
This review is most helpful for practices and health systems, who likely have a mixture of patients from multiple payors.
It must be noted that the process for these exemptions is particularly onerous on the referring provider. Submitting the exemption can be done only by the provider themselves and requires login to the payor specific portal.
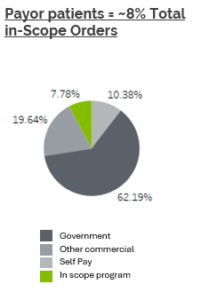
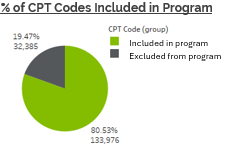
Additionally, while a substantial number of imaging codes are included in the program, the limited number of providers who are eligible, the fact that this program is only for one payor, and the aforementioned submission requirements severely limit the ability of the program to reduce the burden of authorizations.
Bottom Line: Low Expected Impact
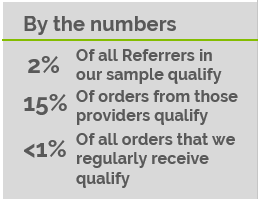
- In our review, less than 1% of orders
received by us would be eligible for exemption, and at that, they would only be exempt if the referring provider was willing to take on ownership of the process of obtaining the exemption.
- We anticipate very low impact on overall authorization needs due to the relatively low number of referrals that qualify, and the administrative burden placed directly on the providers.
- Insurers will likely continue to face pushback on authorization processes as an obstacle for patients and providers
Our team at Centauri Health Solutions is available to answer any questions and to help you navigate changes to the prior authorization processes.
Nate Clark
Director, Client Engagement – RM&A
Centauri Health Solutions, Inc.
 received by us would be eligible for exemption, and at that, they would only be exempt if the referring provider was willing to take on ownership of the process of obtaining the exemption.
received by us would be eligible for exemption, and at that, they would only be exempt if the referring provider was willing to take on ownership of the process of obtaining the exemption.